
In this phase, assessment and treatment priorities focus on the preventable causes of death as defined by military medical evidence: Major Hemorrhage, Airway, Breathing/Respirations, Circulation, and Head & Hypothermia.
Tactical Field Care (TFC) phase: This phase can be initiated once the threat has been addressed and/or the casualty is in a safe location. Care Under Fire (CUF) phase: Wherein the primary concern is any threat to life/safety in the form of enemy fire or environment, as well as utilizing tourniquets to manage massive hemorrhage. The evidence-based approach that motivated the Committee on Tactical Combat Casualty Care (CoTCCC) to adopt the M A R C H mnemonic has drastically changed that approach for the better.Īccording to the TCCC guidelines, there are three phases of care: The old school approach to trauma was: Airway, Breathing, Circulation (ABC). Tactical Combat Casualty Care (TCCC) revolutionized our approach to trauma by utilizing evidence-based medicine in replacing the antiquated ABCs with the MARCH mnemonic. If you are not familiar with MARCH, here is what you need to know. The exact role of angiographic embolization, which should be a life-saving procedure, deserves further study.Stop the Bleed > MARCH Mnemonic and TCCC MARCH Mnemonic and TCCC Tactical Combat Casualty Care (TCCC) revolutionized our approach to trauma by utilizing evidence-based medicine in replacing the antiquated “ABCs” with the MARCH mnemonic. For patients who underwent angiographic embolization, mortality was 54.1%, and for those who suffered a cardiac arrest, mortality was 90%.Ĭonclusion: In blunt trauma patients with hemorrhagic shock who met criteria for the lethal triad on presentation to the ER, angiographic embolization, APACHE II score, and cardiac arrest independently predict mortality. 7.6%, p=0.01), although they had similar laparotomy rates (52.8 % vs. 14.3%, p=0.001) or an operative thoracic procedure (thoracotomy, sternotomy, or VATS, 26.4% vs. Non-survivors were more likely to undergo angiographic embolization (37.7% vs. 3232☒779 mL, p<0.001) and were more likely to have a cardiac arrest (50.9% vs. Compared to survivors, non-survivors were older (46☒2 vs. There was no difference in pre-injury comorbidities, body mass index, Injury Severity Score, multiple organ dysfunction score, ER systolic BP, ER heart rate, ER body temperature, crystalloid volume administered within 12 hours, WBC count, and platelet count between survivors and non-survivors. 
The mean age of the cohort was 39 years, 70% were male, and 90% were White. Results: A total of 172 patients met all three criteria.
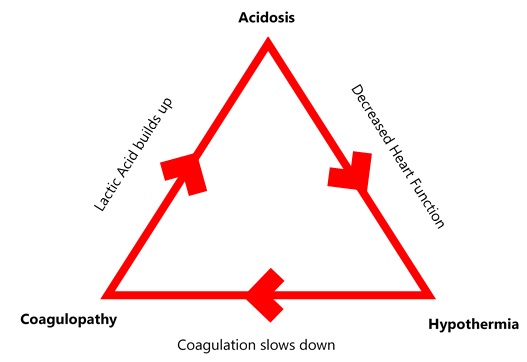
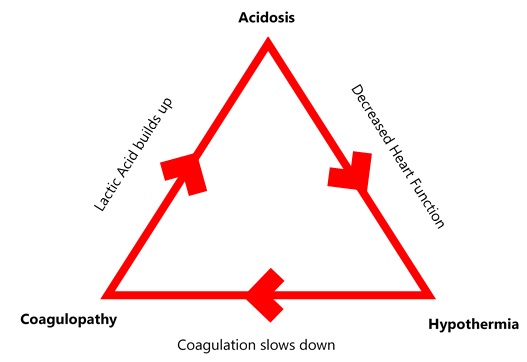
Univariate analyses were used to compare survivors and non-survivors while multivariable analysis was used to determine predictors of mortality. Patients who, on presentation to the emergency room (ER), had the triple combination of severe hyperlactatemia (serum lactate >4 mg/dL), coagulopathy (INR >1.5) and hypothermia (body temperature ≤ 36 ☌) were included. Methods: The Inflammation and the Host Response to Injury database was analyzed. We examine clinical variables that contribute to mortality in blunt traumatic shock patients presenting with this triad. Resuscitation and control of bleeding are two key tenets of trauma care designed to halt this vicious cycle. Introduction: The combination of acidosis, coagulopathy and hypothermia in a trauma patient is a harbinger of death. Siram 1 1Howard University College Of Medicine,Surgery,Washington, DC, USA 2Emory University Hospital,Surgery,Atlanta, GEORGIA, USA 3Northwestern University Feinberg School Of Medicine,Surgery,Chicago, ILLINOIS, USA





 0 kommentar(er)
0 kommentar(er)
